AHCA Invites Medicaid Providers to Shape Re-Procurement as 12 Health Plans Vie for Contracts

AHCA Invites Medicaid Providers to Shape Re-Procurement as 12 Health Plans Vie for Contracts
The Agency for Health Care Administration (AHCA) is inviting input from Medicaid-participating health care providers concerning the Statewide Medicaid Managed Care (SMMC) program re-procurement, as mandated by Section 409.966(3)(a)(8) of Florida Statutes.
Provider feedback is one of the scored criteria that AHCA will consider in its contract award decisions. Submitting comments empowers Medicaid providers to influence program design, policies, and regulations, ultimately enhancing health care delivery to Medicaid recipients and improving accountability within the SMMC program.
Medicaid home health providers should consider submitting comments for several important reasons:
- Advocating for Recipients: Providers often have valuable insights into the needs and challenges of Medicaid recipients. By submitting comments, they can advocate for program improvements that ultimately benefit the individuals they serve.
- Quality of Care: Providers can raise issues related to the quality of care delivered through the program. They can propose changes to ensure that recipients receive appropriate, effective, and timely care.
- Payment and Reimbursement: Providers can address concerns about reimbursement rates, which can impact their ability to deliver services. They can request fair and sustainable payment structures to ensure that they can continue to participate in the program.
- Administrative Processes: Providers can suggest improvements to administrative processes that affect their interactions with the program. This may include streamlining paperwork, reducing administrative burdens, and ensuring efficient claims processing.
- Network Adequacy: Providers can raise concerns about network adequacy. They can advocate for a sufficient number of providers in the network to meet recipient needs, particularly in underserved areas.
- Transparency and Accountability: Providers can request greater transparency in program operations and financial matters. They can advocate for measures that hold managed care organizations (MCOs) accountable for their performance, including quality of care and financial stewardship.
- Cultural Competency and Specialized Care: Providers can advocate for cultural competency training and specialized care for diverse patient populations, ensuring that the program addresses the unique needs of different communities.
- Coordination of Care: Providers can emphasize the importance of care coordination among different health care providers to ensure seamless, comprehensive care for recipients.
- Health Equity: Providers can advocate for measures to address health disparities and promote health equity among Medicaid recipients. This may include addressing social determinants of health and other factors that affect health outcomes.
The details and documents related to this re-procurement, including timelines and instructions for submitting provider comments, can be accessed through the Department of Management Services' (DMS) MyFloridaMarket Place Vendor Information Portal.
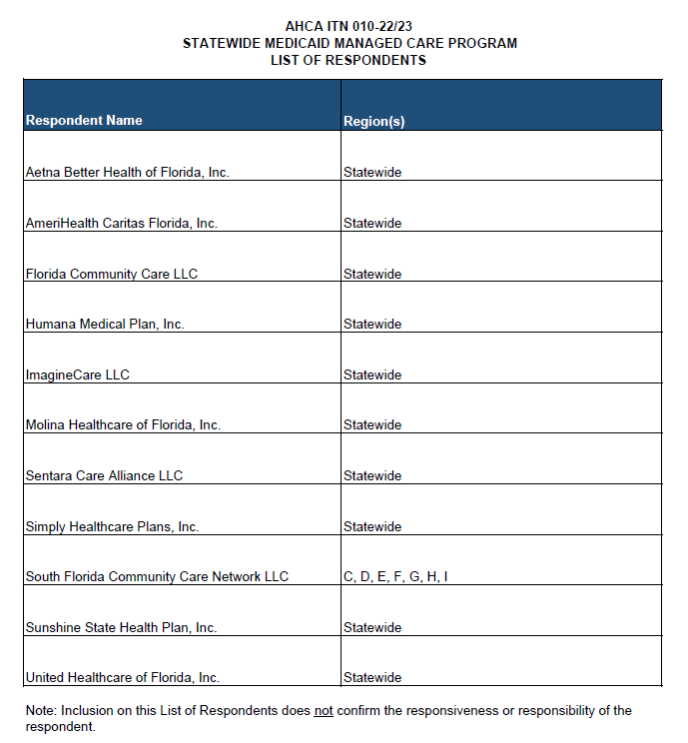
Twelve managed care organizations are competing for Florida Medicaid contracts, as outlined below. Two of the respondents, Sentara Care Alliance (formerly Optima Health) and ImagineCare, do not have existing contracts with the state. The other respondents include Sunshine Health, Aetna Better Health of Florida, Molina Healthcare of Florida, United Healthcare of Florida, Simply Healthcare Plans, South Florida Community Care Network (d/b/a Community Care Plan), Florida Community Care, Humana Medical Plan, and AmeriHealth Caritas of Florida.
The deadline for providers to submit comments is 5:00 PM ET on November 9, 2023. Providers should reference the SMMC program ITN "AHCA ITN 010-22/23" in their comments.